

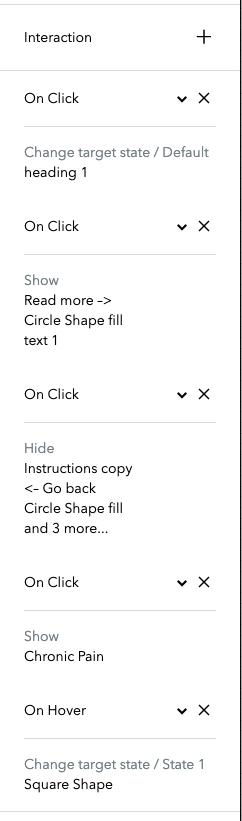
Chronic�pain

Osseointegration prosthesis
Neurotechnology and rehabilitation

Upper-limb
hardware

Manual handling�in care
Rehabilitation
methods
Spinal cord electrical stimulation
Visual prosthesis
and bionic eyes



Issue / challenge:
There are various challenges associated with chronic pain claims due to the subjective and complex nature of pain perception. For example, there are issues associated with quantifying the pain levels that a claimant is experiencing due to a heavy reliance on subjective self-reporting. Additionally, a claimant’s pain and related symptoms, such as sleep disturbance, cognitive issues, and psychological symptoms, are often exacerbated by a lack of understanding about their condition and a lack of personal agency in managing these.
As medical advancements and digital tools evolve, there are ever-increasing ways that these can be utilised in the context of catastrophic injury claims to aid a claimant’s reporting and management of chronic pain and associated symptoms.
Chronic pain
Although these technologies carry the possibility of streamlining the evaluation of pain symptoms, there are also various complications that insurers need to be alive to. For example, the reliance on mobile health data potentially raises concerns about data privacy, the authenticity of the data, and the possibility of data misinterpretation.
Key take away:
Technologies such as wearable devices and health-tracking mobile applications have the capability to strengthen the way that we consider and value pain claims, as well as facilitate claimants’ active participation and, thus, potential improvement in their pain symptoms.
Although the input of experts in pain management will undoubtedly continue to be invaluable in the handling of these claims, these relatively simple and inexpensive technologies represent a significant opportunity to give claimants a more active role in their treatment. They should be utilised with a balanced and proactive approach to achieve the optimal outcome for our clients, as well as the claimants themselves.







Tech driven transformations in catastrophic injury claims
Click on topics to find out more

Implications for insurer:
It may be possible to obtain more accurate and reliable measurements of the pain symptoms that a claimant is experiencing through technologies such as wearable devices. Smartwatches, for example, collect a vast amount of data that can provide insights into a person’s physical health and activity levels before, during, and after an accident by gathering data such as heart rate, exercise levels, and sleep patterns. These can be extremely valuable in creating a clearer and more objective understanding of the claimant’s physical condition and the impact of their symptoms on daily activities, aligning this with their self-reported information.
There are also various mobile applications that sufferers of chronic pain may be able to use to track and manage their symptoms. An important aspect of self-management is the patient's understanding of their condition, for example, by identifying symptom patterns and factors that may alleviate or aggravate their symptoms. These apps can provide this information to patients, allowing them greater control over their symptom identification and management and reducing the need for an extensive and costly multidisciplinary approach.
Osseointegration prosthesis
Issue / challenge:
Osseointegration is an alternative to traditional socket fitting methods for limb loss amputees. It involves the insertion of a titanium implant directly into the bone and extending out of the residual limb to allow direct anchoring of the prosthesis to the stump.
It is a popular choice with patients when it works. A key benefit is the increased feeling of the prosthetic limb touching the ground afforded to the user. Its best use is for those who have difficulties with socket attachment, problems with skin breakdown, or for double amputees.
But there are a number of risks, such as frequent infection requiring long-term antibiotics, loosening or fracture of the titanium rod and ultimately removal of the implant, which may require further shortening of the residual limb.
Implications for insurer:
The cost of osseointegration in the private sector is significant. Whilst the NHS has started providing osseointegration, it is in selected cases only, as currently the technique is not NICE approved.
Claimants may well be tempted by the potential benefits, but consideration needs to be given to whether they are a good candidate for the procedure, particularly as there is a high rate of early complications. A failed procedure would add cost and have a detrimental effect on the claimant, particularly when there are commonly significant psycho-emotional issues present. However, where it is successful, it can lead to improved outcomes in respect of mobility and lead to reduced prosthetics costs, as there is no need for sockets.
Osseointegration is currently more widely used for lower limb loss, and typically for above knee amputations. However, as technologies advance, the greater benefits could be seen in upper limb amputees, particularly when combined with targeted muscle reinnervation (TMR) and bionics, with the potential for a usable prosthetic hand.
Key take away:
The likelihood is that osseointegration is going to be an increasing method of prosthetic attachment. That will certainly be the case if it becomes widely available on the NHS. Indeed, predictions are that it could become standard practice at the time of amputation. Combined with advancements in prosthetics, bionics and TMR, the possibilities for improved functional use are significant. There are potential savings to be made in claims as a consequence. Nonetheless, cutting edge technology always comes at a price, and so reductions in indemnity spend in one area could be wiped out or exceeded in another. This is particularly relevant when considering the cost of providing and maintaining these advanced limbs and the implications of a failed procedure.
Critical for insurers faced with a claimant seeking osseointegration in present claims is to seek input from all relevant experts on suitability, which will include orthopaedic surgeons, prosthetists and potentially psychiatrists, and provide input on direction to any rehabilitation funding, and raise reasoned objections where appropriate.




Neurotechnology and rehabilitation
Issue / challenge:
Many of the lasting effects of traumatic brain injuries are ‘hidden’. Impairments to cognitive function and mental health symptoms cannot be seen and so are not always easily recognised or understood by others. Such symptoms can impact relationships, employment and can often be a barrier to successful rehabilitation following an injury.
One of the challenges of rehabilitating an individual with a traumatic brain injury can be around lack of engagement with traditional rehabilitation techniques. Such issues can lead to decreased motivation and participation and can prevent individuals from achieving the most from their rehabilitation package.
Implications for insurer:
Neurotechnology involves the use of technology to understand, monitor, or influence the brain and nervous system, and new technologies and methods are being trialled to help treat the emotional and cognitive symptoms resulting from a traumatic brain injury.
Neurostimulation and neuromodulation technologies are being researched to improve cognitive functions. Techniques like transcranial direct current stimulation (TDCS) and transcranial magnetic stimulation (TMS) are being explored to boost memory and attention. Both technologies potentially offer new ways to treat cognitive deficits including impairments in memory, attention, and decision-making abilities.
Further, TMS and neurofeedback technologies offer non-invasive treatments that can stimulate specific brain regions associated with mood regulation. TMS may improve symptoms of depression, anxiety and PTSD, and neurofeedback can help individuals regulate and better understand their emotional state, helping to reduce anxiety and enabling a more positive outlook during rehabilitation.
These methods, whilst still in their infancy, could offer alternatives to �traditional therapies like medications, with fewer side effects.
Key take away:
Anything we can do to maximise engagement in the rehabilitation process is a positive outcome. This in turn could help to reduce the life cycle of claims by speeding up recovery, it could also increase engagement with the litigation and most importantly help to achieve the best possible outcome for claimants.
Whilst these technologies are still being researched and developed it is essential that we keep up to date with the advancements in this area and the benefits for claimants whilst tracking the costs of the same. Currently there are mixed reviews about the usefulness of these technologies and it’s important to bear in mind that the use of neurotechnology could also lead to increased costs and claim durations if interventions are ineffective or result in unforeseen side effects. Ethical, privacy and safety concerns will also need to be carefully considered.


Upper-limb hardware
Issue / challenge:
Individuals with upper extremity amputation often either reject or abandon prostheses due to challenges with significant device weight—particularly among myoelectric prostheses—and limited device dexterity, durability, and reliability among both myoelectric and body-powered prostheses. However, with 17 degrees of freedom and more than 100 sensors in the hand and upper arm, the Modular Prosthetic Limb (MPL) is the world’s most sophisticated upper-extremity prosthesis. There are currently six MPLs being used for research purposes across the United States, with four more in development.
Implications for insurer:
The MPL represents a significant advancement in prosthetic technology capable of restoring intuitive dexterous function for individuals with varied levels of upper extremity loss. The upfront costs of the device are likely to be high and it will require careful consideration to decide whether the long-term benefits outweigh the initial expenditure. However, in scenarios where traditional prosthetics are inadequate, the MPL might offer the necessary functionality to restore independence, making it a potential game-changer in prosthetic care.
Key take away:
The rapid advancement of prosthetic technology is outpacing current medical guidelines making it challenging to assess the necessity and appropriateness of new technologies. The improved functionality and comfort may also lead to more individuals opting for amputations, leading to higher claims and financial exposure for insurers.
To effectively manage these risks, it is essential that we remain informed about technological advancements and develop comprehensive strategies for risk mitigation and cost control to ensure we are prepared for the evolving landscape.

Manual handling in care
Issue / challenge:
The care sector is struggling with the rising costs of care and increasing demands on care providers. Technology might offer a solution by making it easier for patients to take care of themselves, as well as easing the burden of mounting workloads on carers.
There have been considerable technological advances in the care sector in recent years, especially with manual handling. This extends to moving or transferring patients as well as moving equipment.
Assisted transfer devices like sit-to-stand lifts give patients some degree of mobility to participate actively in transfers. These devices offer support and assistance, as well as encourage independence and confidence during daily activities. They also protect care providers by avoiding high risk manual handling tasks. Such devices can reduce the carer’s risk of injury and improve the safety and quality of patient care. They can also avoid the need for two carers to transfer patients, if one carer can perform the same task with technological aids.
Advancements in technology have also led to the development of sensor-assisted devices which enhance the safety and efficiency of moving and handling procedures. Sensor-equipped hoists and slings provide real-time data, allowing caregivers to adjust movements and handling tasks to ensure the patient’s comfort and dignity.
Other developments include the use of artificial intelligence in patient assessments to select the right equipment and ensure the care provider is able to perform a particular task safely.
Implications for insurer:
The cost of such technologies will be significant, especially bearing in mind care claims often make up the largest head of loss in a personal injury claim. Rising care rates, high turnover of staff, and problems with supply and demand in the care sector, make the increased use of technology an attractive option in the right case. Managing those costs and reducing indemnity spend while still ensuring a claimant is provided with a high standard of care, is critical for insurers.
The upfront costs of such aids, together with annual maintenance costs and the costs of training carers on the safe use of equipment, must be balanced against the benefit of the more traditional approach to care.
Questions might also be asked as to whether claimants actually want or would use such devices. Increasing use of technology or AI might lead to patients feeling more isolated or lonely, as they miss the personal contact with carers. Conversely, they may feel more empowered if they can use aids or equipment to manage their own transfers or manual handling, instead of feeling reliant on others to do things for them.
Key take away:
The key to success with such technologies is to ensure the right equipment is available for a particular scenario, and that staff are competent and fully trained in using such devices. Efficiency and compassion should be promoted while ensuring the care package is sustainable and affordable. Ethical issues include a patient’s right to refuse the use of mechanical devices, and a preference for the more traditional carer-led approach to care provision.
In the medicolegal setting, parties should try to work collaboratively to structure care �packages which are appropriate to the particular needs of the individual, and are sustainable �in the long term. There is unlikely to be a “one size fits all” solution – what might work �for one patient might be wholly unsuitable for another. Each case, and indeed each �patient, should be considered on its own facts. Continuing advancements in �technology and AI in the care sector, make this a very interesting area to watch.

Rehabilitation methods
Issue / challenge:
Rehabilitation in the context of musculoskeletal injury is largely focused on assessing, diagnosing, and managing musculoskeletal disorders through orthopaedic physiotherapy. It is usually key to restoring function, relieving pain and improving independence with day-to-day activities. Early, appropriate intervention can be hugely beneficial to claimants’ recovery.
Traditional in-person rehabilitation can be expensive, inconvenient, and prolonged, what with transport issues, waiting lists, and clinical staff shortages. Claimants can often lose interest and drop off rehabilitation programmes. Insurers are only too aware of claimants who start a course of treatment but end up cancelling or failing to attend when life gets in the way. Without consistent, sustained rehabilitation, patient outcomes may be poorer, resulting in higher awards of damages.
Implications for insurer:
In recent years, however, technology is beginning to revolutionise physiotherapy. Motion analysis has always been a fundamental part of physiotherapy, informing the clinical diagnosis and treatment programme. Traditionally, it relied on simple, manual observational methods. More recently, marker-based tracking methods have been developed, involving markers placed on the human body to detect and track each joint’s location through the movement. Using multiple cameras, 3D motion information can be tracked on video and analysed. While this may be considered the gold standard, this kind of tracking generally requires expensive, highly specialist equipment.
Technology continues to develop and could profoundly impact rehabilitation for musculoskeletal injuries. Now, using their own smartphone camera and an app to analyse their joint angles, patients can be guided through exercises with live feedback, without the need to visit a physiotherapist in person. The apps use computer vision and machine learning algorithms to provide detailed insights into movements in real-time, correcting patients’ technique where needed. They can also capture objective measurements, which can be used to track recovery more accurately over time, compared with a more subjective traditional physiotherapy assessment. Some of the apps also integrate ‘gamification’ elements, aimed at making performing rehabilitation exercises more engaging and improving patient compliance.
The potential benefits for insurers cannot be overstated. The increased use of app-based therapy would of course significantly reduce claims for physiotherapy costs, as well as associated travel. Crucially, its accessibility should make rehabilitation easier for claimants to engage with, improving their long-term outcomes and increasing their quality of life. The impact on their overall physical and mental health is obvious. From insurers’ perspective that could positively impact on both awards of damages and on costs – with improved prognoses, claim life cycles could also reduce.
Key take away:
These emerging technologies present a significant opportunity to improve patient outcomes. Of course, they are still in their infancy. At this stage, using a smartphone camera and app is unlikely to be able to entirely replace the nuanced clinical judgment of a trained physiotherapist. There are still limitations in accuracy, for example in analysing poor quality video in low lighting, and with increased uptake, we can likely also expect increased concerns over patient privacy and the security of data captured, along with the possibility of an app providing incorrect guidance resulting in further injury or a worsening of the condition. However, as the technology improves, the potential impact of AI in rehabilitation on insurers’ overall indemnity spend cannot be underestimated.

Spinal cord electrical stimulation
Issue / challenge:
One of the main consequences of Spinal Cord Injury (SCI) outside of mobility restrictions is loss of bowel and bladder control. An often quoted anecdote is – if you ask a spinal cord injured patient on day 1 what their primary goal is, it is to walk. If you ask on day 100 it is to be continent. A new research trial by the London Spinal Cord Injury Centre and the Royal National Orthopaedic Hospital has been commissioned to study the effects of electronic spinal cord stimulation (eSCS) on bowel and bladder function in those living with SCI - ImPRESS trial :: Royal National Orthopaedic Hospital
Implications for insurer:
If this trial is successful and eSCS can improve bowel and bladder function then there are both tangible and intangible benefits for those with SCI, and by extension insurers. Incontinence can be a significant barrier to, for example, a return to work for someone who has suffered an SCI. Greater control over bowel and bladder function will allow SC Injured claimants to return to work for longer periods and in a wider number of roles increasing their post-accident working capacity and reducing loss of earnings claims.
Improvements in bladder and bowel control should also lead to savings in the costs associated in the management of the bladder and bowels whether that is in relation to carer time and the cost of pads, washing etc. A less tangible benefit is the psychological improvement likely with increased control over bowel and bladder function. Whilst there might be an improvement in any psychological injury (and a reduction in PSLA) the potentially greater benefit is the improvement in overall wellbeing making an SCI sufferer more likely to be in the correct mental space to consider settlement of a claim at an early stage.
Key take away:
SIA research suggests 72% of SCI sufferers faced bowel management challenges highlighting how important and widespread the issue is. This study is a 12 month one which began in January 2024. The technology (eSCS) is already used in the treatment of chronic pain so is widely understood. ESCS stimulators are widely available so the route to patient benefit is likely to be short. By utilising existing technology in a different setting, it is hoped that significant improvements in a key issue which goes to the heart of quality of life for SCI patients can be made. The obvious benefits to physical and mental health allied with greater dignity for those with SCI can all help to improve function and independence, allowing more fulfilling lives and less reliance on others.

Visual prosthesis and bionic eyes
Issue / challenge:
The development of visual prostheses continues to lag behind advancements in other prosthetic technologies due to the immense complexity of the human visual system. Visual prosthetic devices aim to provide individuals with advanced vision loss a sense of vision and light sensitivity. However, these devices typically offer low-resolution vision and do not fully restore natural sight. Instead, they provide limited visual sensations.
While several types of visual prostheses are available in the UK, the most advanced options, such as retinal prostheses, are typically accessible only through private providers. The NHS currently offers artificial eyes but not advanced visual prosthetic solutions.
A team of researchers at the University of California is working to revolutionise this field by developing a Smart Bionic Eye. This device will integrate artificial intelligence with visual prosthetics to interpret visual data and translate it into meaningful signals for the brain. The aim is to help users identify people, recognise objects, and navigate their environment more effectively. Although the Smart Bionic Eye will not restore natural vision, it is expected to deliver more practical and functional vision. This innovative technology will build upon the existing Orion Prosthesis System, enhanced with artificial intelligence and object recognition features to address the limitations of current devices.
Implications for insurer:
Visual prostheses are less commonly encountered in insurance claims compared to other prosthetic technologies. With limited availability through the NHS, these devices often come at significant costs to insurers. They are typically recommended only for individuals with minimal remaining vision and are not suitable for all candidates due to the complexities of the visual system. As a result, each case must be evaluated on its individual merits.
While visual prostheses can improve a claimant’s quality of life, they do not fully restore natural vision. Therefore, insurers may still face substantial claims for ongoing care, future loss of earnings, and other related expenses.
The Smart Bionic Eye represents a potentially groundbreaking advancement in visual prosthetics. By offering more meaningful restoration of vision than existing devices, it could significantly enhance the independence and quality of life of claimants with advanced vision loss. Over time, this could help reduce overall claim costs. However, as the technology is still in its early stages of development, it may be several years before it becomes available in the UK. The long-term costs and benefits remain uncertain, and only time will reveal its true impact on claims and insurance costs.
Key take away:
Although various types of visual prostheses are currently available, the Smart Bionic Eye has the potential to transform this field. Despite these promising developments, the technology remains challenging, and visual prosthetic advancements continue to trail behind other types of prostheses due to the delicate and complex nature of the eye.
Visual prostheses are relatively rare in insurance claims compared to upper and lower-limb prosthetics. However, ongoing research and advancements in artificial intelligence could change this landscape. Staying informed about technological progress will be critical for understanding the potential implications for claims, including improved claimant quality of life, extended life expectancy, and potential cost benefits for insurers.

Read more –>
<– Go back
Read more –>
<– Go back
Read more –>
<– Go back
Read more –>
<– Go back
Read more –>
<– Go back
Read more –>
<– Go back
Read more –>
<– Go back
Read more –>
<– Go back



Although these technologies carry the possibility of streamlining the evaluation of pain symptoms, there are also various complications that insurers need to be alive to. For example, the reliance on mobile health data potentially raises concerns about data privacy, the authenticity of the data, and the possibility of data misinterpretation.
Key take away:
Technologies such as wearable devices and health-tracking mobile applications have the capability to strengthen the way that we consider and value pain claims, as well as facilitate claimants’ active participation and, thus, potential improvement in their pain symptoms.
Although the input of experts in pain management will undoubtedly continue to be invaluable in the handling of these claims, these relatively simple and inexpensive technologies represent a significant opportunity to give claimants a more active role in their treatment. They should be utilised with a balanced and proactive approach to achieve the optimal outcome for our clients, as well as the claimants themselves.
Issue / challenge:
Individuals with upper extremity amputation often either reject or abandon prostheses due to challenges with significant device weight—particularly among myoelectric prostheses—and limited device dexterity, durability, and reliability among both myoelectric and body-powered prostheses. However, with 17 degrees of freedom and more than 100 sensors in the hand and upper arm, the Modular Prosthetic Limb (MPL) is the world’s most sophisticated upper-extremity prosthesis. There are currently six MPLs being used for research purposes across the United States, with four more in development.
Implications for insurer:
The MPL represents a significant advancement in prosthetic technology capable of restoring intuitive dexterous function for individuals with varied levels of upper extremity loss. The upfront costs of the device are likely to be high and it will require careful consideration to decide whether the long-term benefits outweigh the initial expenditure. However, in scenarios where traditional prosthetics are inadequate, the MPL might offer the necessary functionality to restore independence, making it a potential game-changer in prosthetic care.

The upfront costs of such aids, together with annual maintenance costs and the costs of training carers on the safe use of equipment, must be balanced against the benefit of the more traditional approach to care. Questions might also be asked as to whether claimants actually want or would use such devices. Increasing use of technology or AI might lead to patients feeling more isolated or lonely, as they miss the personal contact with carers. Conversely, they may feel more empowered if they can use aids or equipment to manage their own transfers or manual handling, instead of feeling reliant on others to do things for them.
Key take away:
The key to success with such technologies is to ensure the right equipment is available for a particular scenario, and that staff are competent and fully trained in using such devices. Efficiency and compassion should be promoted while ensuring the care package is sustainable and affordable. Ethical issues include a patient’s right to refuse the use of mechanical devices, and a preference for the more traditional carer-led approach to care provision.
In the medicolegal setting, parties should try to work collaboratively to structure care packages which are appropriate to the particular needs of the individual, and are sustainable in the long term. There is unlikely to be a “one size fits all” solution – what might work for one patient might be wholly unsuitable for another. Each case, and indeed each patient, should be considered on its own facts. Continuing advancements in technology and AI in the care sector, make this a very interesting area to watch.
Read more –>
<– Go back
machine learning algorithms to provide detailed insights into movements in real-time, correcting patients’ technique where needed. They can also capture objective measurements, which can be used to track recovery more accurately over time, compared with a more subjective traditional physiotherapy assessment. Some of the apps also integrate ‘gamification’ elements, aimed at making performing rehabilitation exercises more engaging and improving patient compliance.
The potential benefits for insurers cannot be overstated. The increased use of app-based therapy would of course significantly reduce claims for physiotherapy costs, as well as associated travel. Crucially, its accessibility should make rehabilitation easier for claimants to engage with, improving their long-term outcomes and increasing their quality of life. The impact on their overall physical and mental health is obvious. From insurers’ perspective that could positively impact on both awards of damages and on costs – with improved prognoses, claim life cycles could also reduce.
Key take away:
These emerging technologies present a significant opportunity to improve patient outcomes. Of course, they are still in their infancy. At this stage, using a smartphone camera and app is unlikely to be able to entirely replace the nuanced clinical judgment of a trained physiotherapist. There are still limitations in accuracy, for example in analysing poor quality video in low lighting, and with increased uptake, we can likely also expect increased concerns over patient privacy and the security of data captured, along with the possibility of an app providing incorrect guidance resulting in further injury or a worsening of the condition. However, as the technology improves, the potential impact of AI in rehabilitation on insurers’ overall indemnity spend cannot be underestimated.
Read more –>
<– Go back
Implications for insurer:
Neurotechnology involves the use of technology to understand, monitor, or influence the brain and nervous system, and new technologies and methods are being trialled to help treat the emotional and cognitive symptoms resulting from a traumatic brain injury.
Neurostimulation and neuromodulation technologies are being researched to improve cognitive functions. Techniques like transcranial direct current stimulation (TDCS) and transcranial magnetic stimulation (TMS) are being explored to boost memory and attention. Both technologies potentially offer new ways to treat cognitive deficits including impairments in memory, attention, and decision-making abilities.
Further, TMS and neurofeedback technologies offer non-invasive treatments that can stimulate specific brain regions associated with mood regulation. TMS may improve symptoms of depression, anxiety and PTSD, and neurofeedback can help individuals regulate and better understand their emotional state, helping to reduce anxiety and enabling a more positive outlook during rehabilitation.
These methods, whilst still in their infancy, could offer alternatives to �traditional therapies like medications, with fewer side effects.
Read more –>
<– Go back
Issue / challenge:
One of the main consequences of Spinal Cord Injury (SCI) outside of mobility restrictions is loss of bowel and bladder control. An often quoted anecdote is – if you ask a spinal cord injured patient on day 1 what their primary goal is, it is to walk. If you ask on day 100 it is to be continent. A new research trial by the London Spinal Cord Injury Centre and the Royal National Orthopaedic Hospital has been commissioned to study the effects of electronic spinal cord stimulation (eSCS) on bowel and bladder function in those living with SCI - ImPRESS trial :: Royal National Orthopaedic Hospital
Implications for insurer:
If this trial is successful and eSCS can improve bowel and bladder function then there are both tangible and intangible benefits for those with SCI, and by extension insurers. Incontinence can be a significant barrier to, for example, a return to work for someone who has suffered an SCI. Greater control over bowel and bladder function will allow SC Injured claimants to return to work for longer periods and in a wider number of roles increasing their post-accident working capacity and reducing loss of earnings claims.
Read more –>
<– Go back
Issue / challenge:
The development of visual prostheses continues to lag behind advancements in other prosthetic technologies due to the immense complexity of the human visual system. Visual prosthetic devices aim to provide individuals with advanced vision loss a sense of vision and light sensitivity. However, these devices typically offer low-resolution vision and do not fully restore natural sight. Instead, they provide limited visual sensations.
While several types of visual prostheses are available in the UK, the most advanced options, such as retinal prostheses, are typically accessible only through private providers. The NHS currently offers artificial eyes but not advanced visual prosthetic solutions.
A team of researchers at the University of California is working to revolutionise this field by developing a Smart Bionic Eye. This device will integrate artificial intelligence with visual prosthetics to interpret visual data and translate it into meaningful signals for the brain. The aim is to help users identify people, recognise objects, and navigate their environment more effectively. Although the Smart Bionic Eye will not restore natural vision, it is expected to deliver more practical and functional vision. This innovative technology will build upon the existing Orion Prosthesis System, enhanced with artificial intelligence and object recognition features to address the limitations of current devices.
Read more –>
<– Go back
Osseointegration is currently more widely used for lower limb loss, and typically for above knee amputations. However, as technologies advance, the greater benefits could be seen in upper limb amputees, particularly when combined with targeted muscle reinnervation (TMR) and bionics, with the potential for a usable prosthetic hand.
Key take away:
The likelihood is that osseointegration is going to be an increasing method of prosthetic attachment. That will certainly be the case if it becomes widely available on the NHS. Indeed, predictions are that it could become standard practice at the time of amputation. Combined with advancements in prosthetics, bionics and TMR, the possibilities for improved functional use are significant. There are potential savings to be made in claims as a consequence. Nonetheless, cutting edge technology always comes at a price, and so reductions in indemnity spend in one area could be wiped out or exceeded in another. This is particularly relevant when considering the cost of providing and maintaining these advanced limbs and the implications of a failed procedure.
Critical for insurers faced with a claimant seeking osseointegration in present claims is to seek input from all relevant experts on suitability, which will include orthopaedic surgeons, prosthetists and potentially psychiatrists, and provide input on direction to any rehabilitation funding, and raise reasoned objections where appropriate.
Clyde & Co's catastrophic injury specialists examine issues arising from the use of emerging technology for claimants who have suffered severe injury and have significant ongoing needs.
�
We explore the latest technological developments and highlight the opportunities and challenges for claimants and insurers. These technologies include devices for manual handling, wearable tech for pain management, innovative prosthetics, neurotechnology for brain injuries, AI-driven rehab, and treatments for spinal cord injuries. They also have the potential to improve patient care and independence against a backdrop of rising care costs and increasing demands on care providers.
�
While these technologies hold significant promise, it is important to consider the associated costs, patient suitability, and ethical implications. Successfully implementing these technologies requires a good understanding of the balance between risks and cost savings whilst always being conscious of the impact of their use on vulnerable claimants.