The publication of this article was funded by Bayer

Allergy & Immunology

Climate change is one of the leading causes resulting �in increasing prevalence and complexity of AR
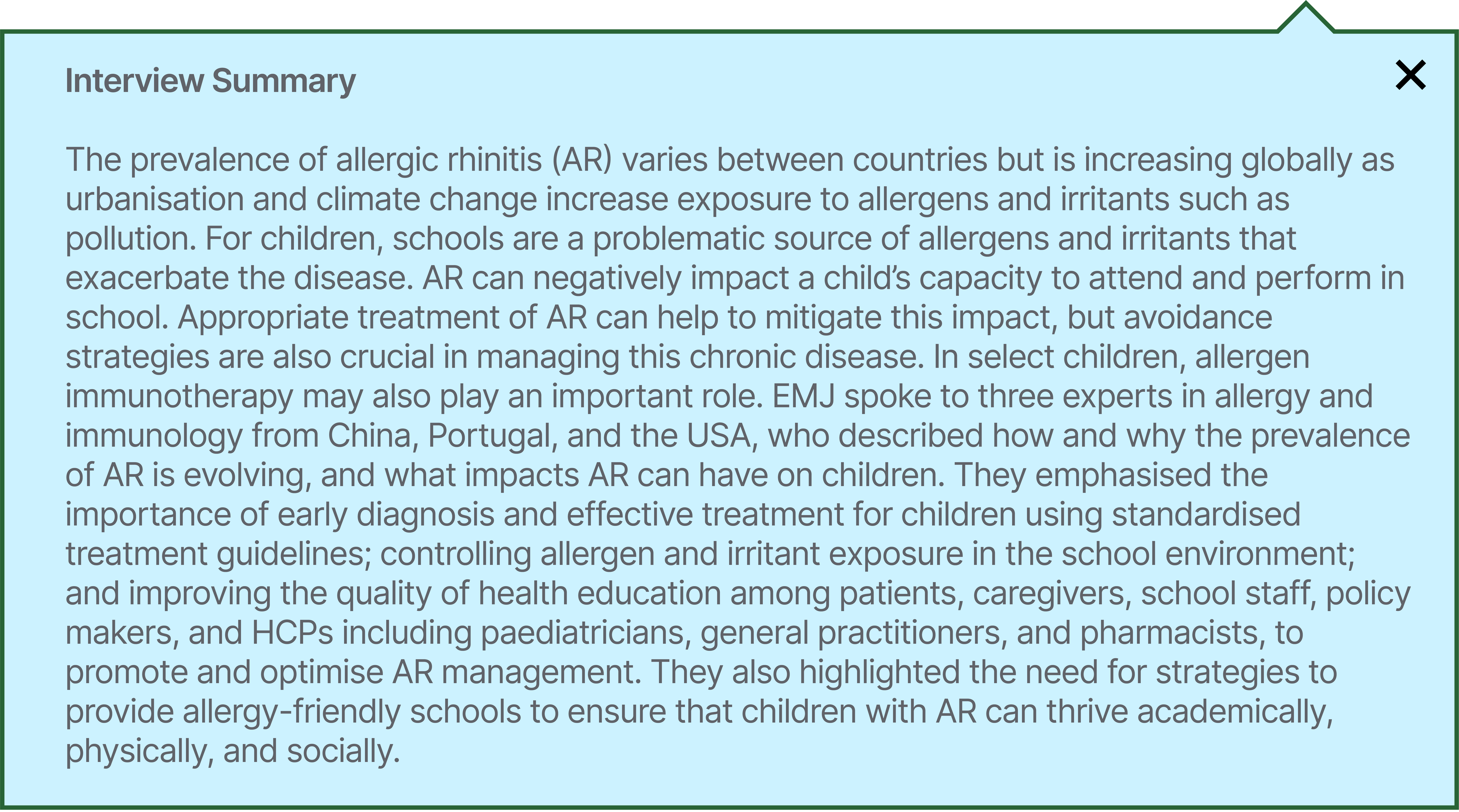
Allergic rhinitis (AR), the most prevalent allergic disease across all age groups, causes a substantial and increasing burden on the health of individuals around the world.
Prevalence data suggest that 10.5–19.9% of children globally suffer from AR.1,2


Global Perspectives on Challenges & Opportunities
in Managing Allergic Rhinitis in Children:
Taking the School Environment as a Case

Disclaimer: The KOLs interviewed in this article were selected and compensated by Bayer, and the manuscript was reviewed by Bayer. Opinions expressed in this article belong solely to the named interviewees.


INTRODUCTION







Increased urbanisation is also driving:
Comorbidities such as asthma are common, and estimates suggest that 80% of people with asthma also have AR, while up to 40% of individuals with AR also have asthma.14
ALLERGIC RHINITIS COMORBIDITIES
80


40
%

Blaiss, Morais-Almeida and Cheng highlighted their observations that the number of children experiencing AR is increasing across the globe.





IMPACT OF ALLERGIC RHINITIS ON CHILDREN
Many schools have inadequate ventilation and aging infrastructure that can increase the presence of allergens, contribute to poor health and detrimental impact to a child's quality of life, including:16




Absenteeism
Symptomatic students missed 2.8x more school days than asymptomatic students.17


The detrimental effects of AR on children can be mitigated through timely and appropriate management of symptoms
EVOLVING PREVALENCE AND SEVERITY
IMPACT OF THE SCHOOL ENVIRONMENT ON PAEDIATRIC ALLERGIC RHINITIS

Poorly controlled AR has been shown to result in lower academic productivity due to AR symptoms, use of sedating antihistamines, poor sleep quality, and increased absenteeism.17


children and adolescents spend much of their time either in their bedroom or the classroom, and while the home environment can be adapted to reduce allergen exposure, the school environment is more difficult for the individual or caregiver to control.










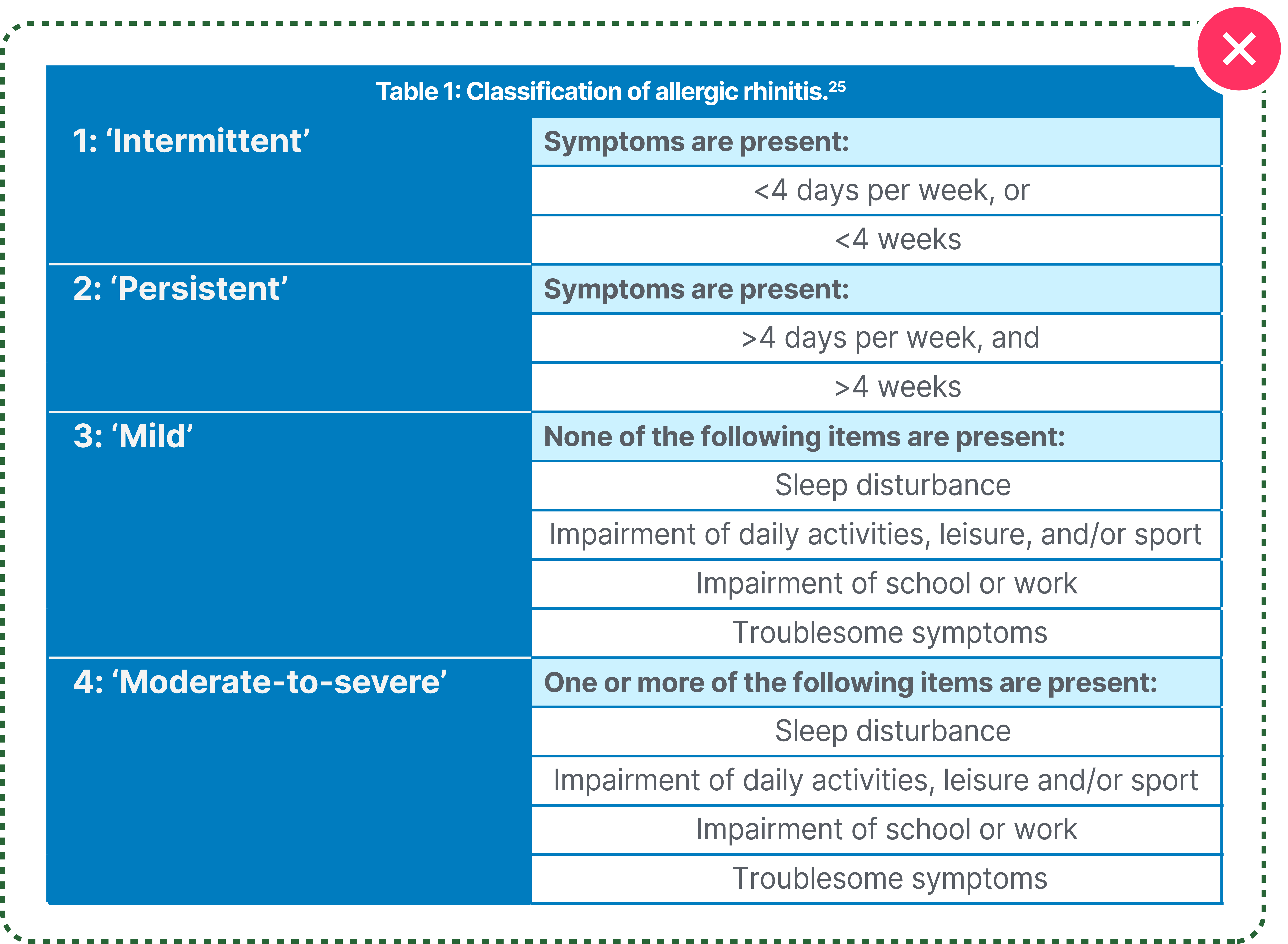
CLASSIFICATION OF ALLERGIC RHINITIS


The diagnosis of AR is based on both the frequency of symptoms and the severity of symptoms.22
In the Allergic Rhinitis and its Impact on Asthma (ARIA) classification guidelines,23 symptoms experienced less than �4 days a week or less than 4 consecutive weeks are considered intermittent, whereas in persistent AR, symptoms last more than �4 days a week and 4 consecutive weeks.24
AR severity is categorised as mild when �there is no impact on daily activities or sleep, �or moderate-to-severe when symptoms interfere with sleep, daily activities, or school, or trigger serious sequelae like asthma attacks (Table 1).25



POORLY CONTROLLED ALLERGIC RHINITIS
Studies show that children with allergic conditions are more likely to be:



Achieving good AR and asthma control can return school performance to normal.28

DEVELOPMENT OF EFFECTIVE ALLERGIC RHINITIS TREATMENT GUIDELINES
Evidence-based guidelines for the treatment of AR are being implemented across the globe. In Europe and the USA, the ARIA guidelines form the basis for the treatment of mild and moderate-to-severe, intermittent, or persistent AR.22,28
The Chinese guidelines, informed by research in China and internationally, align closely with the ARIA guidelines, recommending four types of drugs as first-line treatments for AR, including:15

Studies show that children with allergic conditions are more likely to be:
Oral second-generation antihistamines
Nasal glucocorticoids
Leukotriene receptor antagonists

Nasal antihistamines
In 2022, the updates to the Chinese guidelines included separate guidelines for adults and children that are very specific and easy for HCPs to follow.
Cheng also outlined that the Chinese guidelines follow the principle of combining prevention and treatment, with a ‘four in one’ approach:29




CHALLENGES OF IMPLEMENTING GUIDELINES: �TRIVIALISATION OF ALLERGIC RHINITIS AND RISE OF MISINFORMATION

Despite the availability of evidence-based guidelines for the management of AR, in many cases, AR is not managed efficiently.



In the USA, we are increasingly seeing non-compliance to medication among patients, and lack of understanding of how to use medication.


Blaiss expressed worries that misinformation circulating on social media is exacerbating non-compliance and creating fear among patients.
Many people self-medicate for AR with over-the-counter medications when they might also benefit from consulting an HCP.

OPTIMISING TREATMENTS FOR PAEDIATRIC PATIENTS WITH ALLERGIC RHINITIS
An important element of health education, said Blaiss and Morais-Almeida, is to advise patients and caregivers on the sedative effects of first-generation antihistamines.

Both Blaiss and Morais-Almeida noted first-generation antihistamines no longer have a place in AR treatment, and are not recommended in any AR treatment guidelines, a view that is widely supported by a recent publication in the WAO journal, and others.32,33

ENSURING PROMPT AND EFFECTIVE CONTROL OF ALLERGIC RHINITIS

All three experts highlighted the importance of the role of the HCP to ensure prompt and effective control of potentially comorbidities, in particular asthma AR in children to avoid progression to more severe symptoms and comorbidities, in particular asthma.


Morais-Almeida summarised the point, saying:


It is important to control AR today and next week, to reduce the impact on everyday activities and school performance, but it is also important to treat for the future.

THE IMPORTANCE OF SHARED DECISION-MAKING
Encouraging shared decision-making between children, caregivers, and HCPs is also crucial for successful management of AR, the experts said. Morais-Almeida recommends starting conversations with young patients as early as possible.

When you have the patient and their caregiver in the room, you need to explain the treatment options, and work with them to decide what they find most acceptable. For example, there is no point in prescribing an intranasal corticosteroid if they say they won’t use a nasal spray. The patient is a partner, and you need to agree on what treatment regimen will best suit the patient’s lifestyle.


Blaiss agreed, saying:
Conclusion
Blaiss and Morais-Almeida believe that AR management plans developed in collaboration with caregivers and doctors, similar to the mandatory asthma action plans, would help children with AR to navigate the school environment and empower teachers to support individuals’ needs. Raising awareness of best practices in the management of AR,�including shared decision-making between patients, caregivers, and HCPs, is vital to �improve adherence, quality of life, and treatment outcomes.

Children spend a lot of time at school, so the school environment is one that we need to control.


Cheng agreed, saying:









Abbreviations

References



The global prevalence of physician diagnosed AR has doubled over the last decade1






Knowing the particular allergens in your area and time of pollination is important in limiting outdoor exposure






Many people in Portugal, and other parts of Southern Europe are experiencing persistent AR. This is likely because of the effects of climate change, which is lengthening pollen seasons and increasing air pollution




In China, we have observed a rapid increase in both population-based surveys and hospital-based diagnosis data in the past decades. People affected by self-reported AR increased by almost 100 million in 2011 compared to 20052,15

A meta-analysis of Chinese epidemiological studies of children found that the diagnosed prevalence of allergic rhinitis from 2012–2021 was higher (19.75%) than that from 2001–2011 (14.81%).2,15 “These are astonishing figures,” Cheng said, explaining that increasing urbanisation, pet ownership, and air pollution are driving the AR epidemic.



Presenteeism
Diminished performance while at school. AR resulted in an average of 26% of academic hours lost.18




Social
Symptoms of AR such as rhinorrhoea and sneezing can isolate children with AR from their peers, as well as physical appearance, such as the allergic crease on the nose and infraorbital dark circles, contributing negatively towards social interactions.
Adolescents with AR symptoms reported activity limitations and lack of self-satisfaction twice as often as those without AR symptoms.19



Academic Performance
Both symptoms of AR and poor rhinitis control negatively impact academic productivity and performance.20



Symptoms of AR can cause sleep disturbances.
Children with AR symptoms report �sleep disturbances 2.5x more often �than those without.19
Sleep




The experts agreed that better education for HCPs, caregivers, and patients would improve awareness of AR and its triggers, help to reduce the detrimental impact of AR symptoms and suboptimal medication, and support better quality of life and academic performance for young people. �The experts also agreed that more should be done to help reduce exposure to allergens in the school environment.



The impacts of uncontrolled AR on children are significant. Sleep disruption, sneezing, and rhino-conjunctivitis make it difficult for children to concentrate and function as normal during the day. Children who experience AR symptoms, or need to take medication at school, also often have feelings of social isolation and self-consciousness.20




The experts believe that teachers and school staff need to be better informed about the impact AR can have on their students, and what mitigation strategies can be put in place.
Environmental control measures are important to reduce allergen exposure in school, including the choice of trees planted in the grounds and procedures for cleaning classrooms.


Often classrooms are cleaned and then closed at the end of the day without any ventilation, exposing children to irritants the following morning, said Morais- Almeida. We need to focus on air quality.




Poor air filtration can contribute to higher levels of allergens and irritants in the classroom.
Air filtration can reduce PM2.5 exposure for children by 75%.12
A 2018 study across 66 classrooms in China found indoor PM2.5, PM10, CO, HCHO, bacteria and fungi GM concentration were 47.40 μg/m3, 72.91 μg/m3, 0.37 mg/m3, 0.02 mg/m3, 347.51 CFU/m,3 and 362.76 CFU/m3, respectively.11
% of classrooms exceeding guideline values for:
PM2.5

66.5%
%
PM10


CO2
Open windows in the classroom can allow pollen and other outdoor allergens to enter the classroom.

Mould, rodents, and cockroaches
Cockroach and mouse allergens are commonly detected in classroom dust samples of urban schools.21
Action: Implementing an integrated pest management approach can help reduce these exposures.21


The number of pet owners in the classroom is one of the strongest predictors of elevated cat and dog allergens in the schools.21
Action: One study showed that having dedicated school clothing has been shown �to reduce airborne pet dander by 4-6x.21


Some cleaning products can act as irritants, particularly for children with allergic conditions.
Action: Usage of allergy-friendly cleaning products.

Action: Replacing soft furnishing with surfaces that are easier to clean and keep dust and allergen free.

Soft furnishing such as carpets and curtains can harbour higher levels of dust mites and other allergens.21



In a lower quartile for reading ability23�
Can be at increased risk of bullying and victimisation compared to children without respiratory conditions.26,27

AR symptoms may start with an itchy nose and sneezing, but can develop to nasal obstruction, persistent cough, and sleep disruption.

Morais-Almeida explained that, often, when patients go to the doctors to talk about their AR symptoms, they end up focusing on other conditions or symptoms, such as experiencing a high number of respiratory infections, restless sleep, snoring, and headaches.




These medicines cause drowsiness and have other potentially harmful side-effects in a significant percentage of our population, including in the paediatric age group.
This is problematic for children, impacting their ability to concentrate in school, and for adults where, for example, the sedation impairs driving performance and psychomotor function, including reaction time.31



First-line care for mild intermittent or persistent, and moderate-to-severe intermittent AR includes second-generation antihistamines, and addition or replacement with nasal corticosteroids when symptoms are not controlled.2,8



Cheng emphasised the need to use second-generation antihistamines to minimise sedation and other cognitive adverse events.

For the treatment of AR in children, non-sedating second-generation antihistamines are recommended to avoid central nervous system inhibition that may affect cognitive function





He continued: “In patients with moderate-to-severe and persistent AR, we would recommend combining second generation antihistamines with intranasal corticosteroids that have low systemic bioavailability because it is important to ensure growth is not affected, especially when some children with persistent AR require corticosteroids for 12 weeks or more.”



1. Licari A et al. Epidemiology of allergic rhinitis in children: a systematic review and meta-analysis. J Allergy Clin Immunol Pract. 2023;11(8):2547-56.
2. Wang RK et al. Prevalence of allergic rhinitis in Chinese children from 2001 to 2021: meta analysis. Chin J Prev Med. 2022;56(6):784-93.
3. Schreurs W et al. 25-year retrospective longitudinal study on seasonal allergic rhinitis associations with air temperature in general practice. NPJ Prim Care Respir Med. 2022;DOI:10.1038/ s41533-022-00319-2.
4. Reinmuth-Selzle K et al. Air pollution and climate change effects on allergies in the anthropocene: abundance, interaction, and modification of allergens and adjuvants. Environ Sci Technol. 2017;22:51(8): 4119-41.
5. Wayne P et al. Production of allergenic pollen by ragweed (Ambrosia artemisiifolia L.) is increased in CO2-enriched atmospheres. Ann Allergy Asthma Immunol. 2002;88(3):279-82.
6. D'Amato G. Effects of climatic changes and urban air pollution on the rising trends of respiratory allergy and asthma. Multidiscip Respir Med. 2011;6(1):28-37.
7. Chen Z et al. The association between high ambient air pollution exposure and respiratory health of young children: a cross-sectional study in Jinan, China. Sci Total Environ. 2019;656:740-9.
8. Blaiss et al. The burden of allergic rhinitis and allergic rhinoconjunctivitis on adolescents: a literature review. Ann Allergy Asthma Immunol. 2018;121(1):43-52.e3.
9. Zhao Z et al. Asthmatic symptoms among pupils in relation to winter indoor and outdoor air pollution in schools in Taiyuan, China. Environ Health Perspect. 2008;116(1):90-7.
10. Annesi-Maesano I et al. Poor air quality in classrooms related to asthma and rhinitis in primary schoolchildren of the French 6 cities study. Thorax. 2012;67:682-8.
11. Zhu Y et al. Indoor air quality in the primary school of China-results from CIEHS 2018 study. Environ Pollut. 2021;291:118094.



12. Barkjohn KK et al. Children’s microenvironmental exposure to PM2.5 and ozone and the impact of indoor air filtration. J Expo Sci Environ Epidemiol. 2020;30:971-80.
13. Kreger M et al. An underpinning of school inequities: asthma absences and lost revenue in California schools. J Sch Health. 2020;90(3):200-11.
14. Egan M et al. Allergic rhinitis: the “Ghost Diagnosis” in patients with asthma. Asthma Res Pract. 2015;1:8.
15. Cheng L et al. Chinese Society of Allergy Guidelines for diagnosis and treatment of allergic rhinitis. Allergy Asthma Immunol Res. 2018;10(4):300-53.
16. Wu TD et al. Association of school infrastructure on health and achievement among children with asthma. Acad Pediatr. 2023;23(4):814-20.
17. Sánchez J et al. Adherence to pharmacotherapy improves school performance in children with rhinitis and asthma. Allergol Immunopathol (Madr). 2018;46:467-71.
18. Vieira RJ et al. Impact of allergic rhinitis on academic performance in adolescents and adults: a bayesian analysis of MASK-air® real-world direct patient data. JIACI. 2024;34(6):409-11.
19. Meltzer EO. Quality of life in adults and children with allergic rhinitis. J Allergy Clin Immunol. 2001;108(Suppl 1):S45-53.
20. Walker S et al. Seasonal allergic rhinitis is associated with a detrimental effect on examination performance in United Kingdom teenagers: case-control study. J Allergy Clin Immunol. 2007;120(2):381-7.
21. Esty, B. Asthma and allergies in the school environment. Clin Rev Allergy Immunol. 2019;57(3):415-26.
22. Bousquet J et al. Next-generation Allergic Rhinitis and Its Impact on Asthma (ARIA) guidelines for allergic rhinitis based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) and real-world evidence. J Allergy Clin Immunol. 2020;145(1):70-80.e3. Erratum in: J Allergy Clin Immunol. 2022;149(6):2180.



23. Bousquet J et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008. Allergy. 2008;63:8-160
24. Bousquet J et al. Allergic Rhinitis and its Impact on Asthma (ARIA): achievements in 10 years and future needs. J Allergy Clin Immunol. 2012;13(5):1049-62.
25. Bousquet J et al. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001;108(5):S147-334.
26. Meltzer EO et al. Burden of allergic rhinitis: results from the pediatric allergies in America survey. J Allergy Clin Immunol. 2009;124(3):S43-70.
27. Sánchez J et al. Adherence to pharmacotherapy improves school performance in children with rhinitis and asthma. Allergol Immunopathol (Madr). 2018;46(5):467-71.
28. Scadding GK et al. Allergic rhinitis in childhood and the new EUFOREA algorithm. Front Allergy. 2021;2:706589.
29. Zhang M et al. Highlights of the treatment of allergic rhinitis according to Chinese guidelines. Curr Opin Allergy Clinical Immunol. 2023;23(4):334-40.
30. Klimek L et al.. ARIA guideline 2019: treatment of allergic rhinitis in the German health system. Allergo Journal International. 2019;28
31. Bierly JJ, D'Orazio AL. Hydroxyzine in impaired driving investigations. J Anal Toxicol. 2025;23:bkaf030.
32. Clark JH Let al. Diphenhydramine: it is time to say a final goodbye. World Allergy Organ J. 2025;18(2):101027.
33. Fein MN et al. CSACI position statement: newer generation H1-antihistamines are safer than first-generation H1-antihistamines and should be the first-line antihistamines for the treatment of allergic rhinitis and urticaria. Allergy Asthma Clin Immunol. 2019;15:61.

AR: allergic rhinitis; ARIA: Allergic Rhinitis and its Impact on Asthma, CO2: carbon dioxide; WAO: World Allergy Organisation; HCP: healthcare professional; HCHO: formaldeyhyde; PM: particulate matter; CFU-GM: granulocyte-macrophage colonies in culture.



52.6%
22.4%


Michael Blaiss
Medical College of Georgia at Augusta University, USA
Mário Morais-Almeida
Hospital CUF Descobertas, �Lisbon, Portugal
Lei Cheng
The First Affiliated Hospital with Nanjing Medical University, China

HCHO: formaldehyde concentrations
Poor air filtration can contribute to higher levels of allergens and irritants in the classroom.
Action: Use and regular maintenance of air filtration systems can help to improve the air quality in the school.





Action: When pollen counts are high, keep windows closed, and allow children with pollen allergies to stay inside during outdoor breaks.