Improve patient lives and the delivery of healthcare with our disease prediction service using data insights to uncover patterns in care teams, care delivery and care outcomes.
Huron Intelligence™
Analytic Suite in Healthcare

Request an Assessment
Request an Assessment
Login
Login

Our Analytic Suite Users Include:



We provide the tools you need to improve the quality of care while lowering the costs. Eliminate blind spots so you can protect and grow revenue through new patient acquisition and improved physician alignment.
Organizations want happy, healthy, and productive members. We provide a clear view of your population's health and the risks they individually face, while helping you lower costs and improve the quality of care they receive.
We work with consultants, life sciences companies, software / product vendors, market research / financial services firms, and more who benefit from using our robust data and analytics to illuminate opportunities to achieve their goals.
Payors

Hospitals, Health Systems, and Physician Group Practices
As a healthcare provider, you are focused on the lives of your patients, but you are under ever-intensifying pressure to grow. Not being able to see or predict trends in community health limits your ability to do either. You may have a lot of data, but it is often incomplete or lacking context to reveal insights that you need.
Our platform lets you see and interact with the current picture of your referrals and the clinical pathways taken by your patients. When the current picture is paired with a predictive element, you can visualize the strategic steps you can take to maximize community well-being as well as revenue.
We bring together the industry’s most complete clinical data framework and extraordinary analytical expertise to create the most powerful analytics platform available. Our intuitive tools provide the insights delivered directly to you at the moment you need them.
Analytics for Healthcare Providers
Self Insured Employers, Insurance Brokers, Benefits Consultants, Risk Management
Payors want engaged, activated, and loyal customers. We provide a clear view of your member population's health and the risks they face, while helping lower costs and improving the quality of care they receive.
Our prediction models can highlight a member's risk for the diseases and conditions that have the greatest impact on cost, performance, and their experience.
By connecting the dots between our physician comparison data and individual disease prediction, we can optimize your member population's journey
by matching future needs to the best providers.
This leads to lowered costs, improved care, and increased satisfaction.
Analytics for Healthcare Payors
Reduce costs and improve quality by optimizing care networks with our VOCAL physician scoring application
Reduce costs by predicting which members are at high risk for many diseases and connect with them for low cost screenings
Define and improve consumer journeys by selecting optimal providers in care management. Measure and trend the risk of diagnosis of diseases/conditions across your entire population
Intervene early for members who are rising in risk can lead to better outcomes and lower overall costs of care
Huron Intelligence™ Analytic Suite
enables you to:
Healthcare Consultants, Software/Product Vendors, Financial Services, Market Research
We can provide data exports or API feeds to:
We work with companies that share our desire to improve the delivery of healthcare and the quality of people's lives. With our robust medical claims data set and analytics platforms, we help with strategic initiatives, such as:
Augment your population health system with data
on rising risk trending and disease prediction scoring
Import referral volumes (number of patients and visits)
and physician loyalty scores to PRM and referral
management systems
Get targeted information based on claims data to
better help with business development efforts
Create and manage service line definitions within
your PRM application with our CODE API
Analytics for Other Organizations
Patient Engagement
Provider Network Optimization
Referral Management/Analysis
Digital Front Door Strategy
Risk Stratification / Rising Risk Trending
Disease Prediction
Value Based Pricing / Value Based Care
Financial Services & Market Research Firms:
Objectively value physician practices and other organizations for M&A opportunities
Benchmark diagnosis and procedure volumes for any market in the U.S.
Benchmark utilization data for providers nationwide
Working with the Best
Microsoft
Integrations including Dynamics 365
AWS
Disease Prediction models with Amazon Web Services
Innovaccer
Physician scoring at the point of referral
Salesforce
Delivering insights into your existing workflow
Request an Assessment
Request an Assessment
Back to Top

TEAM

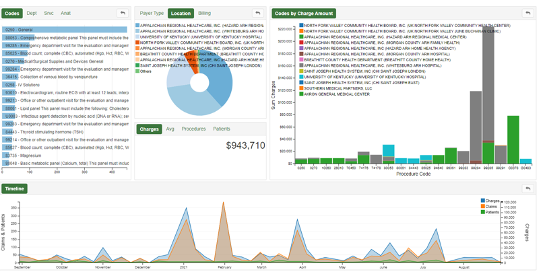
Protect and grow revenue, improve provider alignment, and increase your market share using the TEAM solution. See a complete picture of what’s happening in your market, for both your organization and competitors.
PREDICT

Spot indicators of disease before diagnosis. Quickly analyze billions of medical claims to identify risk factors of early disease onset or surgical procedure. Diagnose and treat earlier to improve the quality of life for patients and families.
VOCAL

Through the use of percentiles and comparisons within the confines of consistent but specific specialties and disease states, VOCAL can provide data-backed views across five important dimensions to expand your view of current provider comparisons.
Providers
Other Organizations
Perception Health
This enterprise subscription enables
users to conduct market share analysis, leakage assessments, referral mapping, disease risk modeling, care pathway analysis
and service line forecasting.
Insights as a Service

Data scientists answer customer questions, integrating Huron, customer and third-party data into models and data visualizations simplifying strategic planning, aiding prioritization and accelerating decisions that impact outcomes.
Consulting Capabilities

We help design strategies to capitalize
on opportunities or address gaps identified through ongoing platform analysis in areas such as capacity planning, consumerism, access optimization, value-based care contracting, and network design.
Data Integrations & Managed Services

Remove barriers to execution with application programming interfaces (APIs) to integrate platform intelligence directly into customer electronic health record, customer relationship management, partner relationship management, and enterprise data warehouse systems — in addition to data analyst, physician coaching, and contact center leader services.

